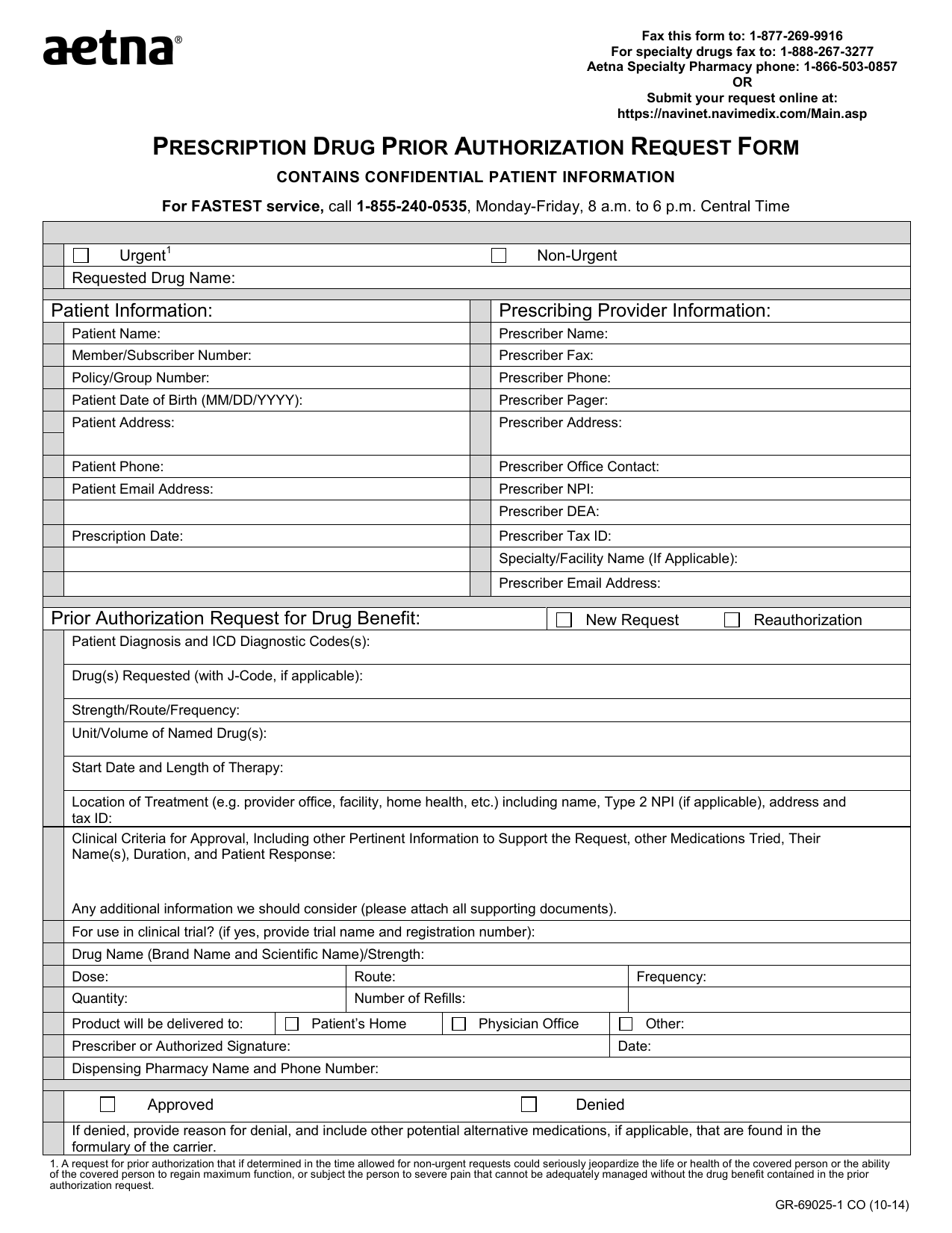
Aetna Medication Prior Authorization Form
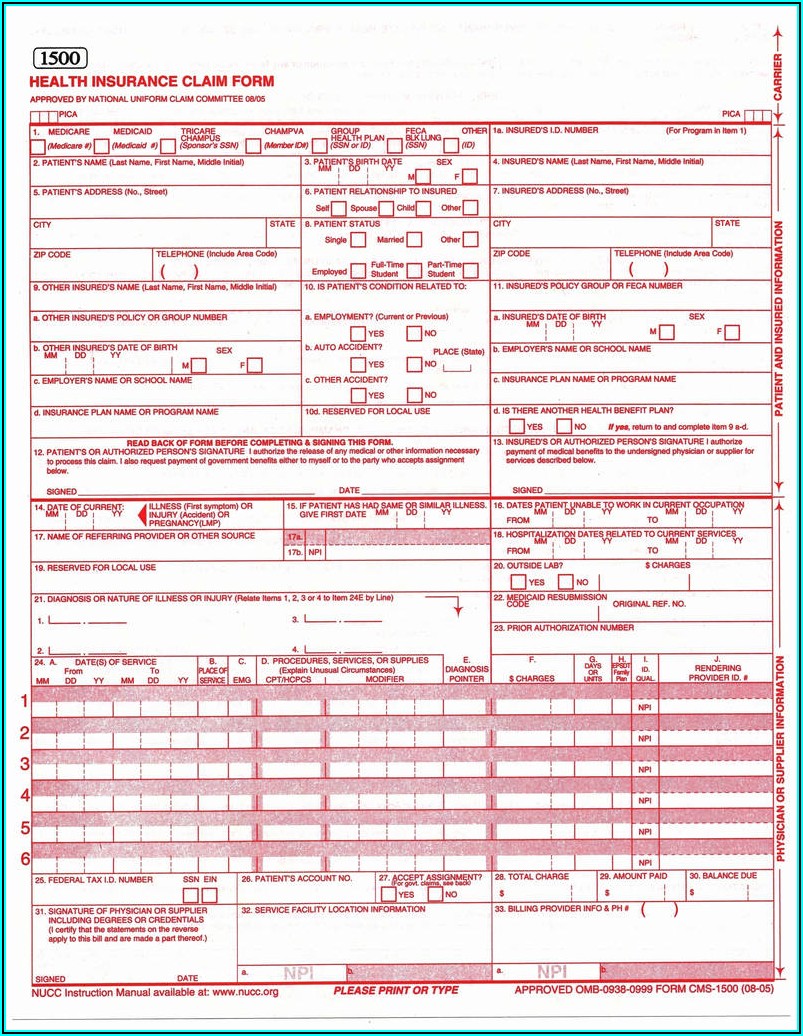
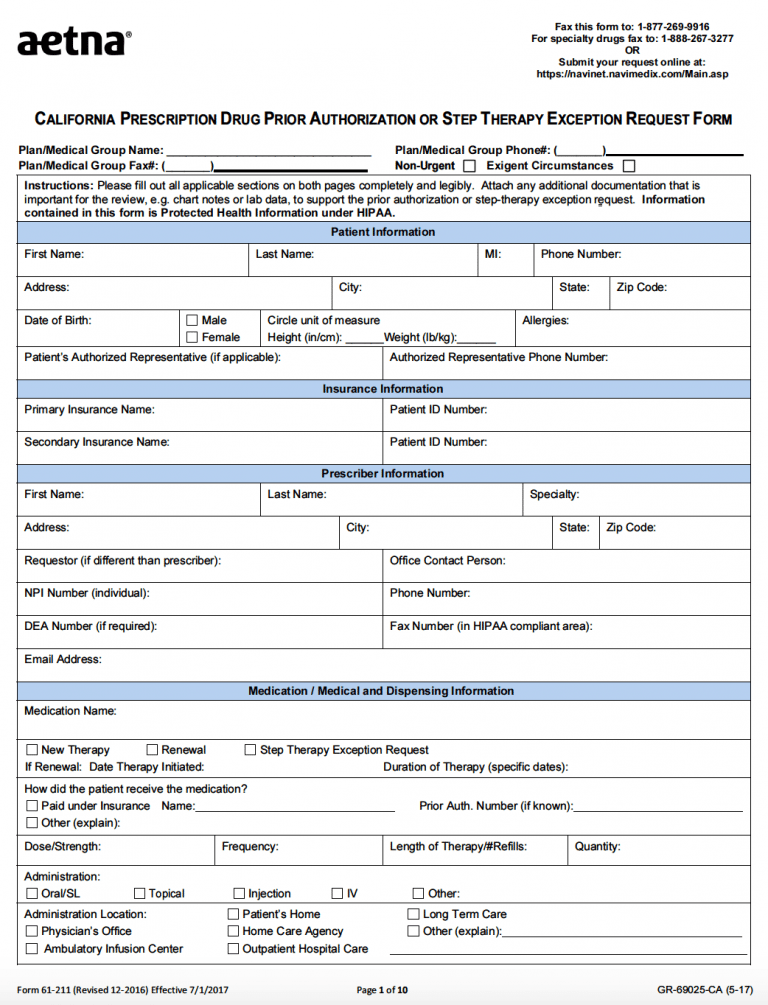
Aetna Medication Prior Authorization Form - Web aetna better health℠ premier plan requires prior authorization for select services. Please attach all clinical information. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web get information about aetna’s precertification requirements, including precertification lists and criteria for patient insurance preauthorization. Web 2023 request for medicare prescription drug coverage determination page 1 of 2 (you must complete both pages.) fax completed form to: Some drugs have coverage rules you need to follow. Adv you can enroll two different ways: For medicare advantage part b: Web enroll now getting started with epa is free and easy. Submit your request online at:
Page 2 of 2 (all fields must be completed and legible for precertification review) aetna precertification. Prior authorization some drugs require you or your physician to get prior. For medicare advantage part b: Adv you can enroll two different ways: Web 2023 request for medicare prescription drug coverage determination page 1 of 2 (you must complete both pages.) fax completed form to: Submit your request online at: Web medication precertification request page 1 of 2 aetna precertification notification. Web prior authorization form all fields on this form are required. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. We know pa requests are complex.
We know pa requests are complex. Web prior authorization form all fields on this form are required. Web enroll now getting started with epa is free and easy. Please attach all clinical information. Web the formulary will tell you if your drug has one of these requirements, such as: Aetna is the brand name used for products and services provided by one or more of the aetna group of companies, including aetna life insurance company and its. You or your doctor needs. Adv you can enroll two different ways: Web aetna better health℠ premier plan requires prior authorization for select services. Web medication precertification request page 1 of 2 aetna precertification notification.
Download AETNA Prescription Drug Authorization Request Form PDF RTF
Prior authorization some drugs require you or your physician to get prior. (denosumab) injectable medication precertification request. Web medicare precertification medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests. Adv you can enroll two different ways: We know pa requests are complex.
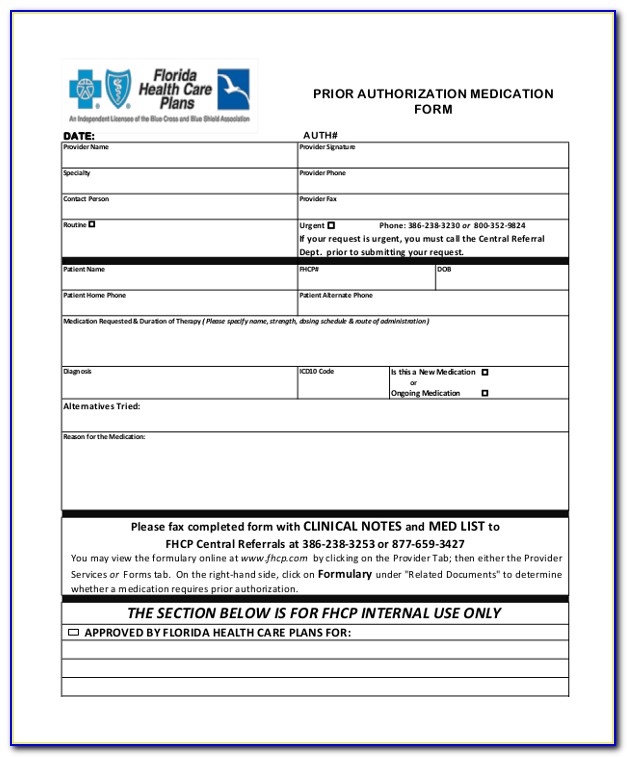
KY Aetna Pharmacy Prior Authorization Request Form Fill and Sign
Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web medication precertification request page 1 of 2 aetna precertification notification. Web the formulary will tell you if your drug has one of these requirements, such as: (denosumab) injectable medication precertification request. Web get information about aetna’s precertification requirements, including precertification lists and criteria.
Aetna Medicare Waiver Of Liability Form Form Resume Examples
Web prior authorization, quantity limits & step therapy. In these cases, your doctor can submit a request on your behalf to get that. Submit your request online at: Web 2023 request for medicare prescription drug coverage determination page 1 of 2 (you must complete both pages.) fax completed form to: However, prior authorization is not required for emergency services.
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web prior authorization form all fields on this form are required. Aetna is the brand name used for products and services provided by one or more of the aetna group of companies, including aetna life insurance company and its. In these cases, your doctor.
Top 6 Aetna Prior Authorization Form Templates free to download in PDF
Web enroll now getting started with epa is free and easy. Web prior authorization form all fields on this form are required. Web medicare precertification medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests. Web get information about aetna’s precertification requirements, including precertification lists and criteria for patient insurance preauthorization. In these.
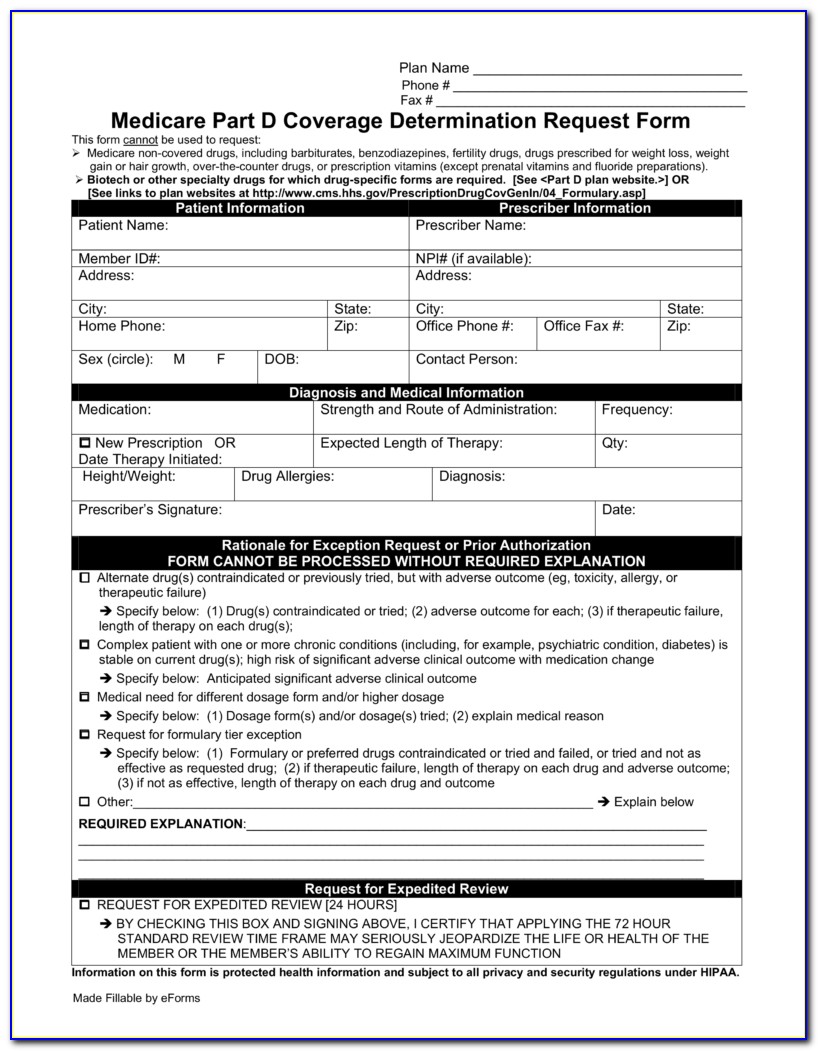
Aetna Medicare Part D Medication Prior Authorization Form Form
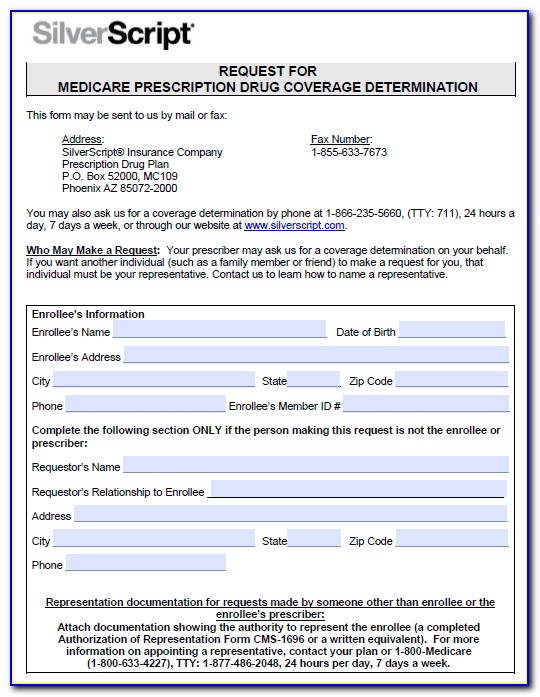
Web 2023 request for medicare prescription drug coverage determination page 1 of 2 (you must complete both pages.) fax completed form to: Aetna is the brand name used for products and services provided by one or more of the aetna group of companies, including aetna life insurance company and its. Please attach all clinical information. For medicare advantage part b:.
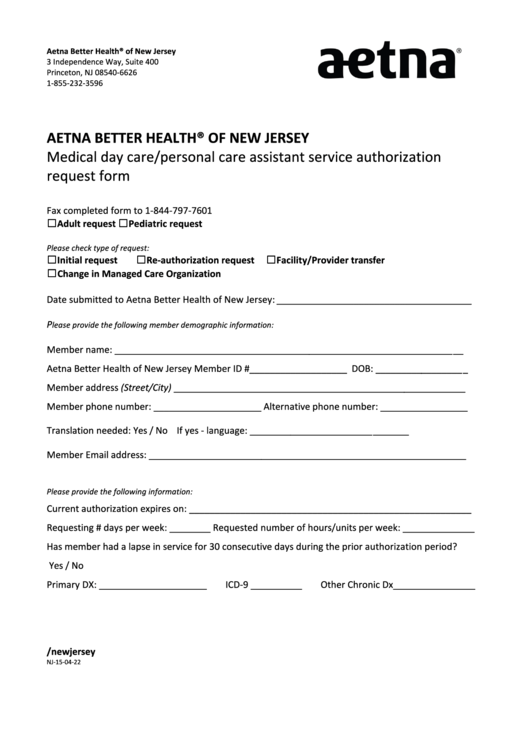
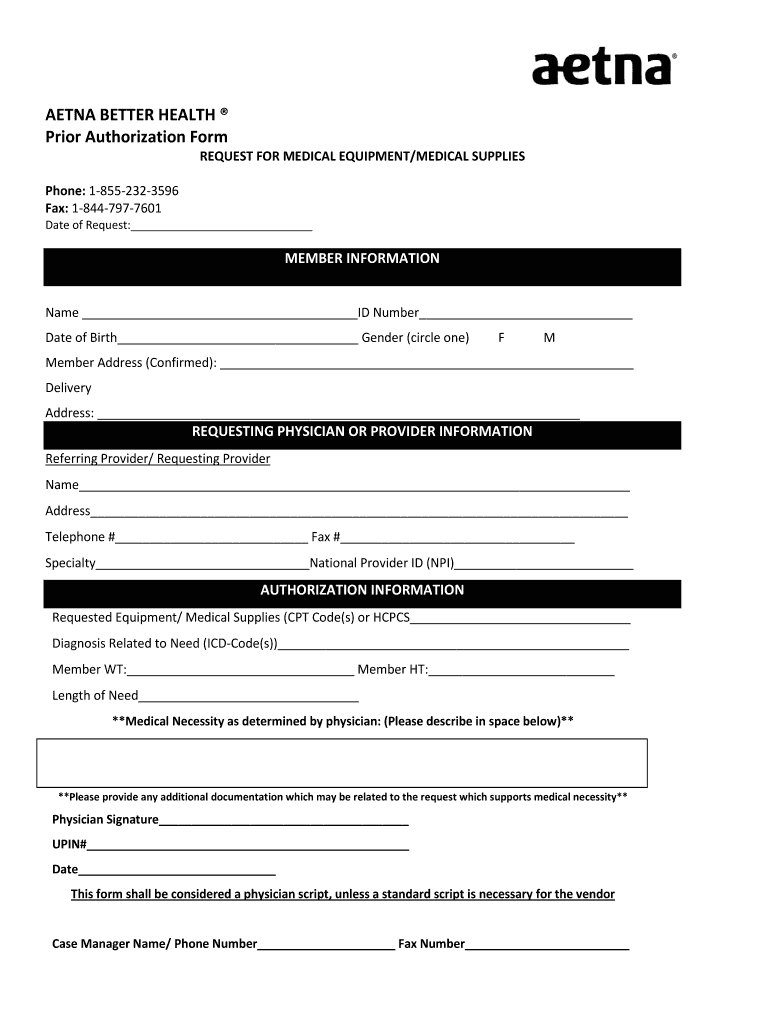
Aetna Better Health Prior Authorization Fill and Sign Printable
However, prior authorization is not required for emergency services. Submit your request online at: You’ll need this info to enroll: Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web aetna provides certain management services to these entities.
Wellcare Medicare Medication Prior Authorization Form Form Resume
In these cases, your doctor can submit a request on your behalf to get that. Web aetna better health℠ premier plan requires prior authorization for select services. Adv you can enroll two different ways: Web medication precertification request page 1 of 2 aetna precertification notification. Web prior authorization, quantity limits & step therapy.
Aetna Medicare Medication Prior Authorization Form Form Resume
Prior authorization some drugs require you or your physician to get prior. Web aetna better health℠ premier plan requires prior authorization for select services. (denosumab) injectable medication precertification request. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web get information about aetna’s precertification requirements, including precertification lists and criteria for patient insurance.
Free AETNA Prior Prescription (Rx) Authorization Form PDF
We know pa requests are complex. Web 2023 request for medicare prescription drug coverage determination page 1 of 2 (you must complete both pages.) fax completed form to: Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Prior authorization some drugs require you or your physician to get prior. Submit your request online.
Web Aetna Provides Certain Management Services To These Entities.
You or your doctor needs. Some drugs have coverage rules you need to follow. Prior authorization some drugs require you or your physician to get prior. However, prior authorization is not required for emergency services.
Please Attach All Clinical Information.
Page 2 of 2 (all fields must be completed and legible for precertification review) aetna precertification. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. For medicare advantage part b: Web 2023 request for medicare prescription drug coverage determination page 1 of 2 (you must complete both pages.) fax completed form to:
Submit Your Request Online At:
In these cases, your doctor can submit a request on your behalf to get that. Web prior authorization, quantity limits & step therapy. You’ll need this info to enroll: Web medication precertification request page 1 of 2 aetna precertification notification.
Adv You Can Enroll Two Different Ways:
Aetna is the brand name used for products and services provided by one or more of the aetna group of companies, including aetna life insurance company and its. Web prior authorization form all fields on this form are required. Web aetna better health℠ premier plan requires prior authorization for select services. Web the formulary will tell you if your drug has one of these requirements, such as: