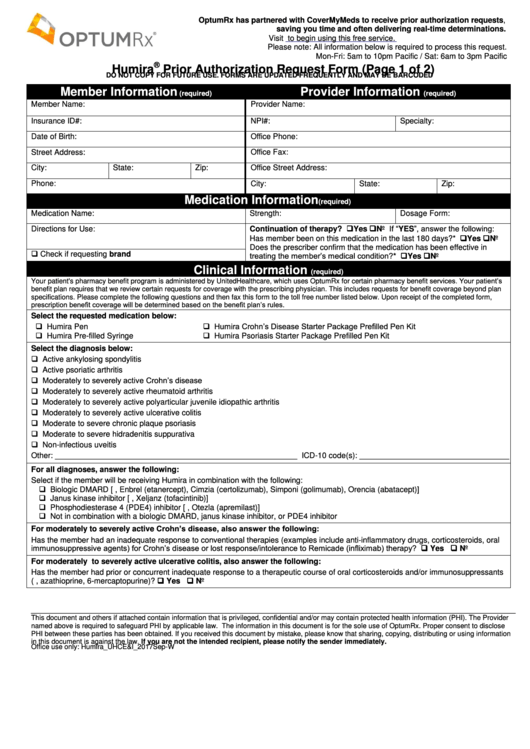
Cvs Caremark Humira Prior Authorization Form
Cvs Caremark Humira Prior Authorization Form - Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Are often injectable or infused medicines, but may also include oral medicines. It could involve accessing personal data, receiving medical treatment, or performing financial transactions. Download the prescribing information for humira®. Web cvs caremark has made submitting pas easier and more convenient. Ad see full safety & prescribing info, & boxed warning. Rheumatoid arthritis (ra) for initial requests: By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Web updated june 02, 2022.
Require additional education of the member and close monitoring of their clinical response in collaboration with their doctor. Are used in the management of specific chronic or genetic conditions. Web formulary exception/prior authorization request form expedited/urgent review requested: Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Ad view benefits, risks, full safety & prescribing info, and boxed warning. A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Prior authorization can ensure proper patient selection, dosage, drug administration and duration of selected drugs. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. It could involve accessing personal data, receiving medical treatment, or performing financial transactions. Web submission of the following information is necessary to initiate the prior authorization review:
Web cvs caremark has made submitting pas easier and more convenient. Web formulary exception/prior authorization request form expedited/urgent review requested: Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Require additional education of the member and close monitoring of their clinical response in collaboration with their doctor. It could involve accessing personal data, receiving medical treatment, or performing financial transactions. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Ad see full safety & prescribing info, & boxed warning. Are often injectable or infused medicines, but may also include oral medicines. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function.
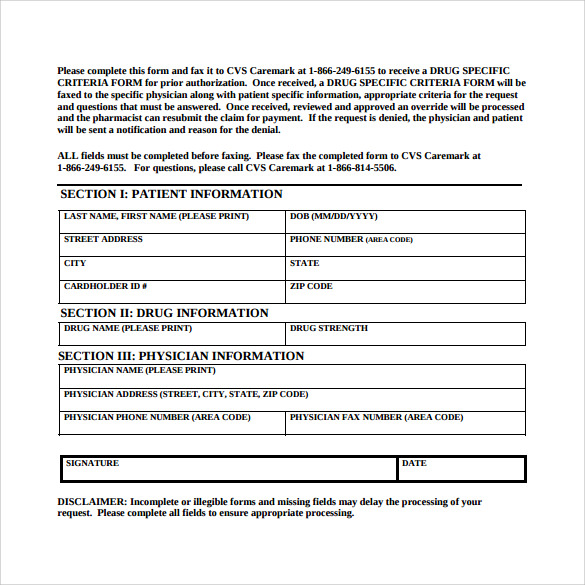
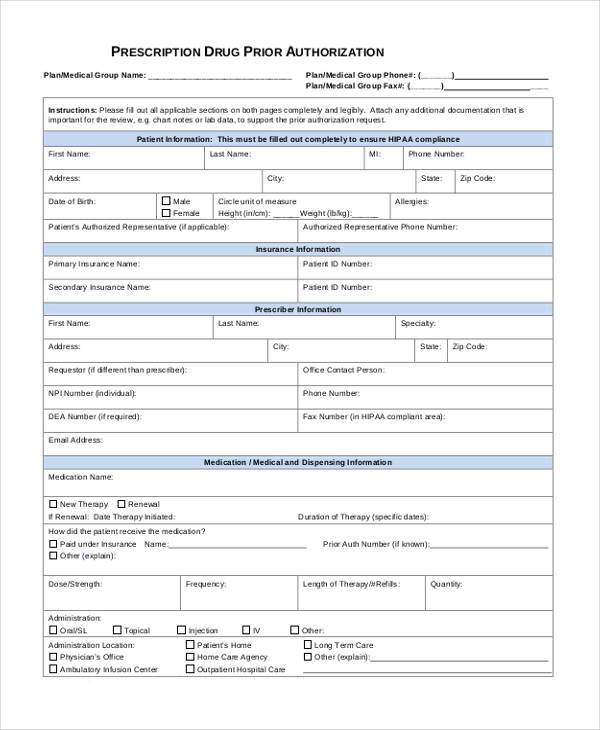
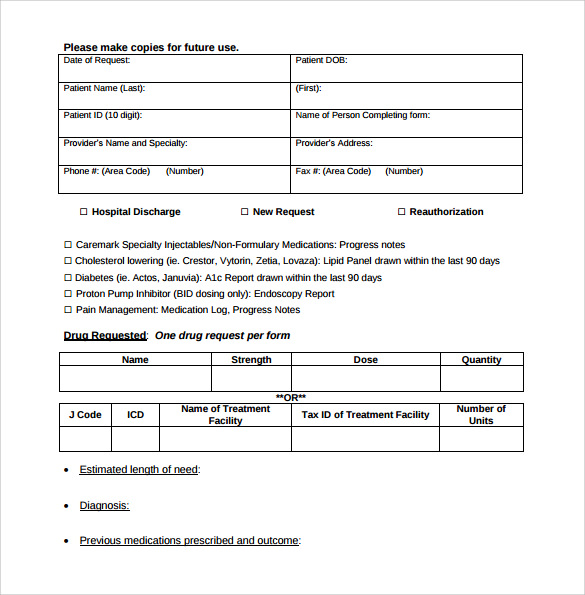
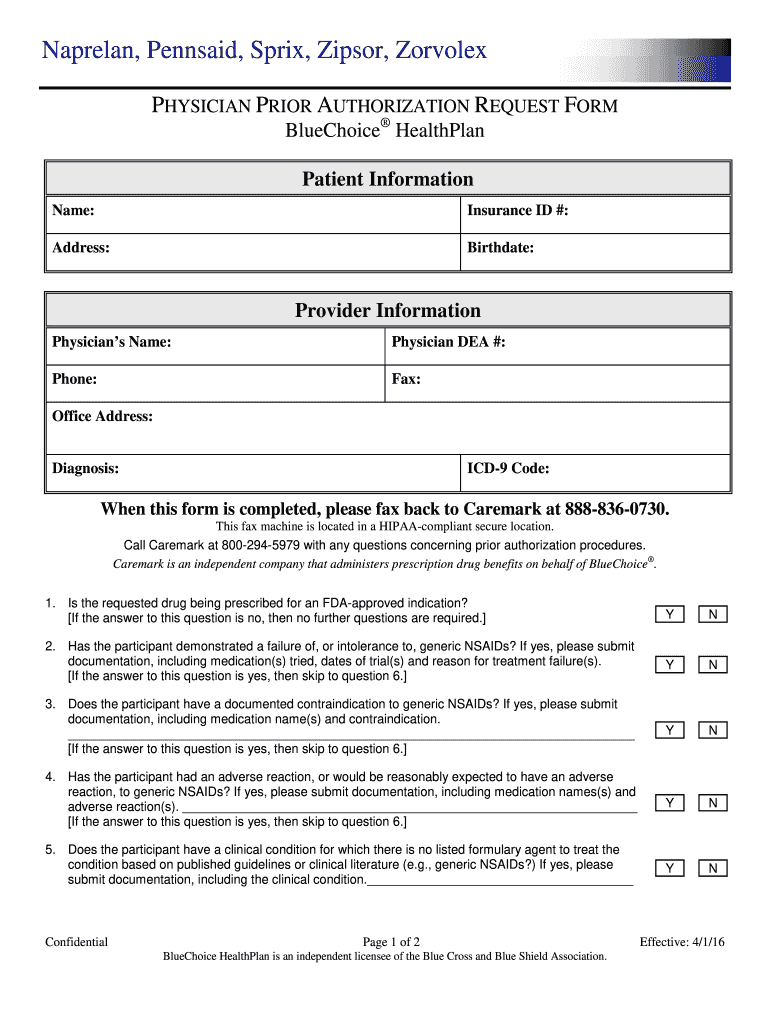
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Ad see full safety & prescribing info, & boxed warning. Require additional education of the member and close monitoring of their clinical response in collaboration with their doctor. We've partnered with covermymeds ® and surescripts ® , making it easy for.
FREE 41+ Authorization Forms in PDF Excel MS word
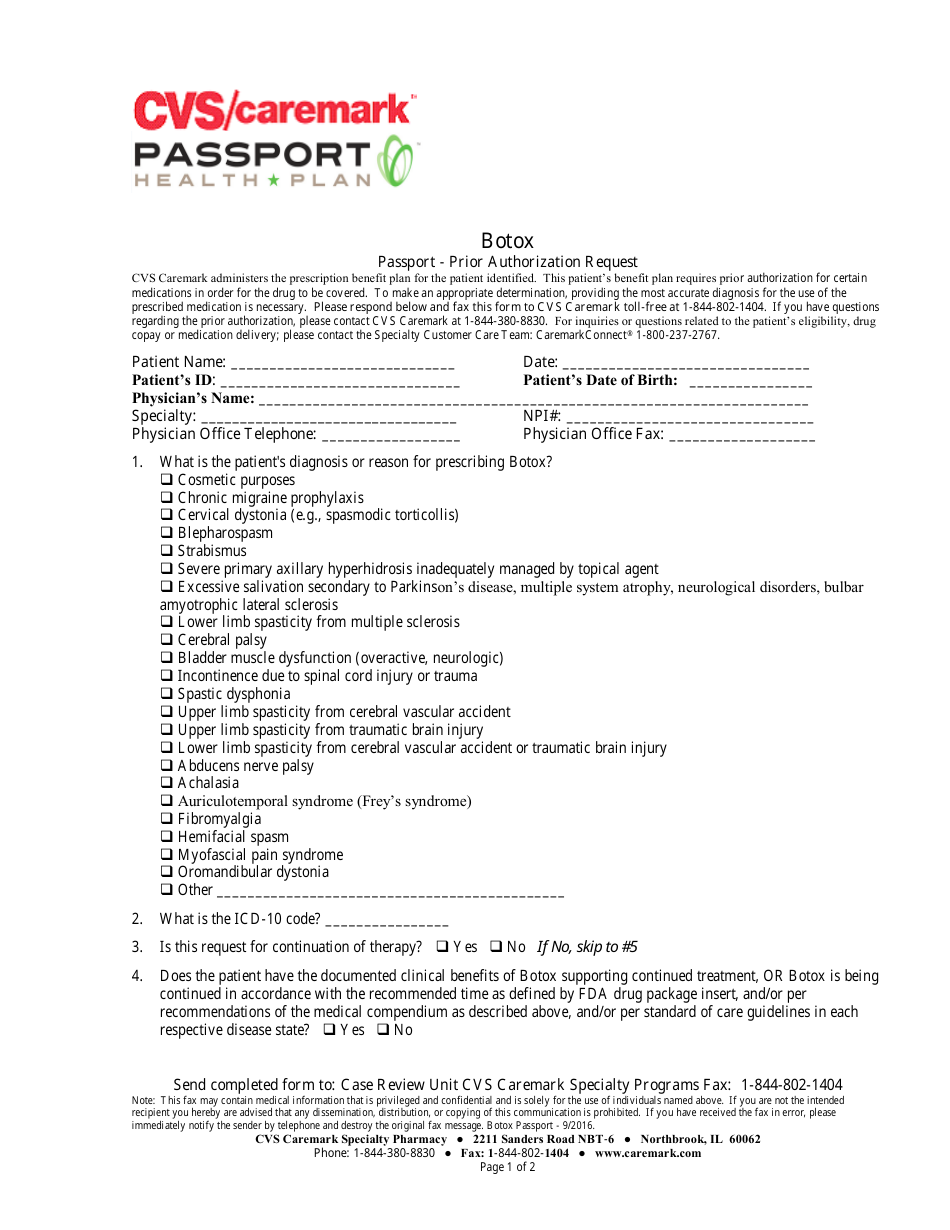
Rheumatoid arthritis (ra) for initial requests: Are used in the management of specific chronic or genetic conditions. Prior authorization can ensure proper patient selection, dosage, drug administration and duration of selected drugs. Web updated june 02, 2022. To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary.
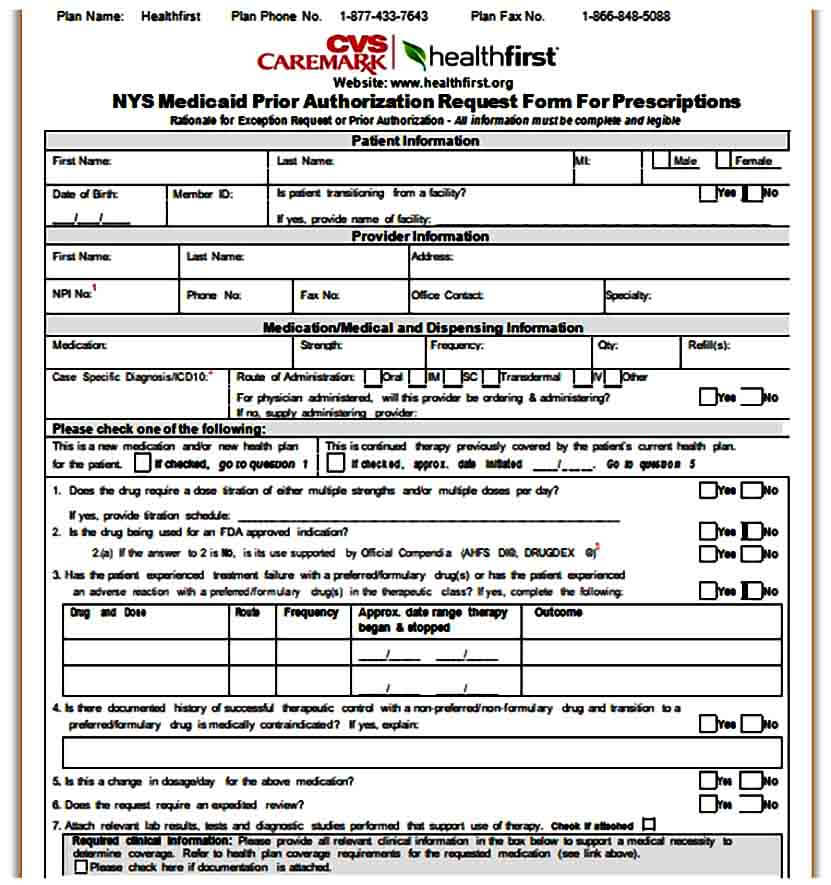
Botox Passport Prior Authorization Request Form Cvs Caremark
It could involve accessing personal data, receiving medical treatment, or performing financial transactions. Web submission of the following information is necessary to initiate the prior authorization review: Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Are used in the management of specific chronic or genetic conditions. By checking this.
cvscaremarkpriorauthorizationform600x800 Free Job Application Form
A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Ad view benefits, risks, full safety & prescribing info, and boxed warning. Web updated june 02, 2022. Download the prescribing information for humira®. Web submission of the following information is necessary to initiate the prior authorization review:
Cvs Caremark Appeal Form Fill Out and Sign Printable PDF Template
Require additional education of the member and close monitoring of their clinical response in collaboration with their doctor. Web submission of the following information is necessary to initiate the prior authorization review: Are often injectable or infused medicines, but may also include oral medicines. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug.
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Require additional education of the member and close monitoring of their clinical response in collaboration with their doctor. Web cvs caremark has made submitting pas easier and more convenient. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician.
Info Caremark Epa Form Fill Out and Sign Printable PDF Template signNow
Rheumatoid arthritis (ra) for initial requests: Download the prescribing information for humira®. Some automated decisions may be communicated in less than 6 seconds! Web formulary exception/prior authorization request form expedited/urgent review requested: To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary.
Humira Prior Authorization Request Form printable pdf download
Web cvs caremark has made submitting pas easier and more convenient. By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Ad see full safety & prescribing info, & boxed warning. Web submission of the following.
Cvs Caremark Formulary Exception Prior Authorization Request Form
Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Web formulary exception/prior authorization request form expedited/urgent review requested: Ad view benefits, risks, full safety & prescribing info, and boxed warning. Are often.
Template Caremark Prior Authorization Form Mous Syusa
To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Ad view benefits, risks, full safety & prescribing info, and boxed warning. Require additional education of the member and close monitoring of their clinical response in collaboration with their doctor. Are used in the management of specific chronic or genetic conditions..
Web Submission Of The Following Information Is Necessary To Initiate The Prior Authorization Review:
Web formulary exception/prior authorization request form expedited/urgent review requested: Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Ad view benefits, risks, full safety & prescribing info, and boxed warning. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage.
Download The Prescribing Information For Humira®.
Are often injectable or infused medicines, but may also include oral medicines. Are used in the management of specific chronic or genetic conditions. Web cvs caremark has made submitting pas easier and more convenient. A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription.
By Checking This Box And Signing Below, I Certify That Applying The Standard Review Time Frame May Seriously Jeopardize The Life Or Health Of The Patient Or The Patient’s Ability To Regain Maximum Function.
Complete/review information, sign and date. Some automated decisions may be communicated in less than 6 seconds! Rheumatoid arthritis (ra) for initial requests: Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered.
Ad See Full Safety & Prescribing Info, & Boxed Warning.
To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web updated june 02, 2022. It could involve accessing personal data, receiving medical treatment, or performing financial transactions. Prior authorization can ensure proper patient selection, dosage, drug administration and duration of selected drugs.