Highmark Bcbs Of Pennsylvania Prior Auth Form
Highmark Bcbs Of Pennsylvania Prior Auth Form - Blood disorders medication request form. Web requiring authorization pharmacy policy search message center. Cgrp inhibitors medication request form. Highmark blue cross blue shield, highmark choice company, highmark health. Web pharmacy prior authorization forms. Web assignment of major medical claim form authorization for behavioral health providers to release medical information designation of authorized. Highmark blue cross blue shield serves the 29 counties of. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization: Highmark blue cross blue shield serves the 29 counties of. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in.
Agents used for fibromyalgia (e.g. Highmark blue cross blue shield, highmark choice company, highmark health. Highmark blue cross blue shield serves the 29 counties of western pennsylvania and 13 counties of northeastern. Cgrp inhibitors medication request form. Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication. Highmark blue cross blue shield serves the 29 counties of. Web assignment of major medical claim form authorization for behavioral health providers to release medical information designation of authorized. Web how to request prior authorization/notification. If you do not yet. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in.
Highmark blue cross blue shield serves the 29 counties of western pennsylvania and 13 counties of northeastern. Blood disorders medication request form. Highmark blue cross blue shield, highmark choice company, highmark health. Web all provider faqs are updated with the most recent information. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization: Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Agents used for fibromyalgia (e.g. Using navinet is the preferred way to request prior authorization/notification from nia. Web requiring authorization pharmacy policy search message center. Complete and fax all requested information below including any supporting documentation as applicable to highmark health.
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication. Web requiring authorization pharmacy policy search message center. Using navinet is the preferred way to request prior authorization/notification.
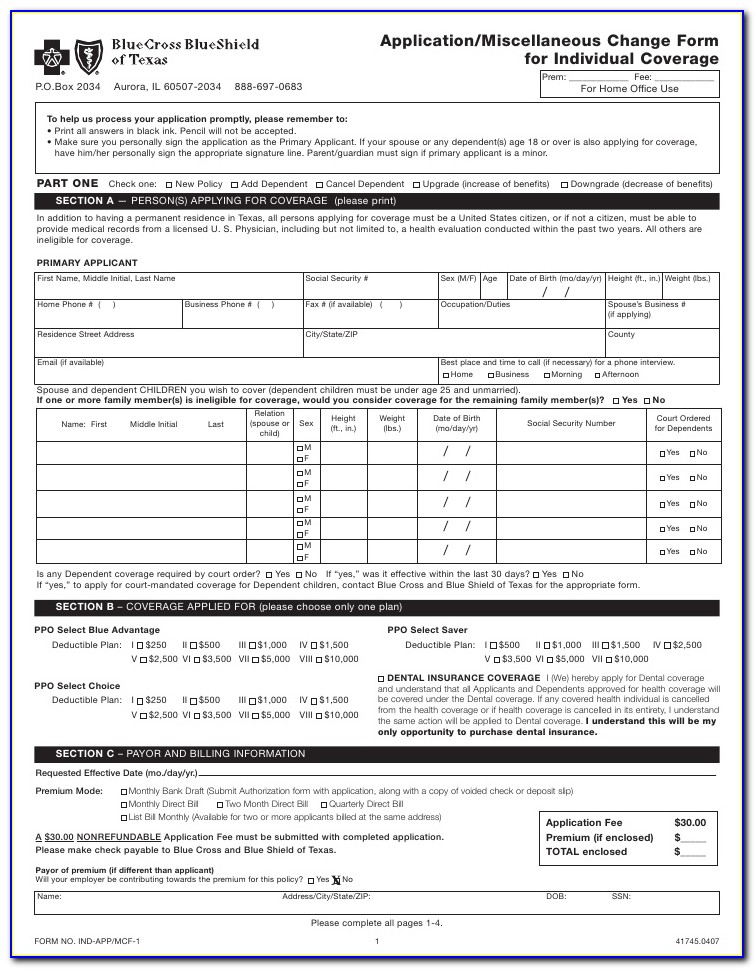
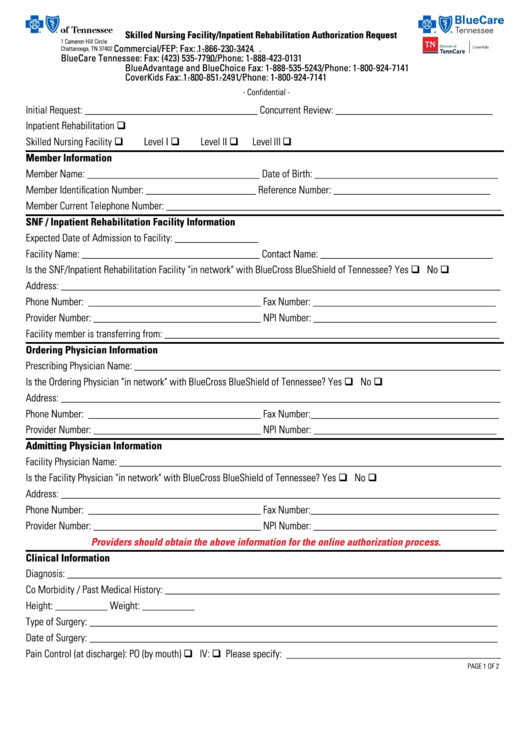
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication. Highmark blue cross blue shield serves the 29 counties of western pennsylvania and 13 counties of northeastern. Web requiring authorization pharmacy policy search message center. Complete and fax all requested information below including any supporting documentation as applicable to highmark health..
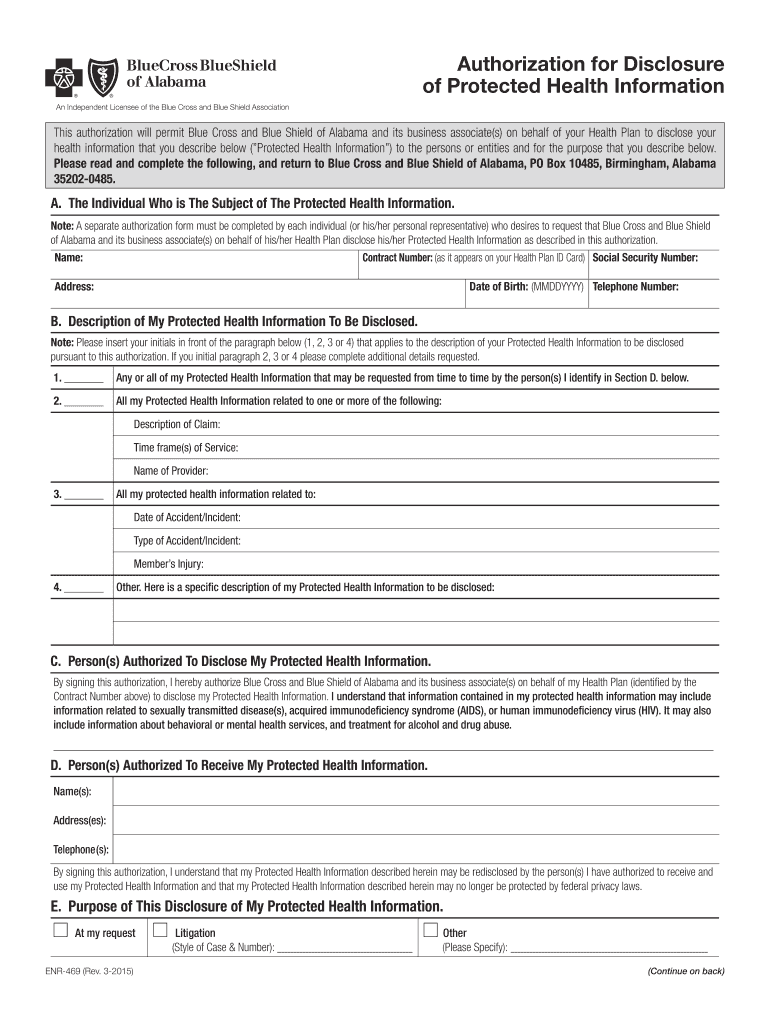
20152022 AL BCBS Form ENR469 Fill Online, Printable, Fillable, Blank
Web how to request prior authorization/notification. Web assignment of major medical claim form authorization for behavioral health providers to release medical information designation of authorized. Web review and download prior authorization forms review medication information and download pharmacy prior authorization forms as a reminder, third. Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form.
Blue cross blue shield pennsylvania highmark availity
Web independent blue cross blue shield plans. Web assignment of major medical claim form authorization for behavioral health providers to release medical information designation of authorized. Blood disorders medication request form. Web requiring authorization pharmacy policy search message center. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13.
ads/responsive.txt Highmark Bcbs Medication Prior Authorization form
Web independent blue cross blue shield plans. Highmark blue cross blue shield serves the 29 counties of. Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication. Blood disorders medication request form. If you do not yet.
Highmark Bcbs Medication Prior Authorization form Lovely Anthem Express
Highmark blue cross blue shield serves the 29 counties of. Precertification prior to admission a preliminary treatment plan and discharge plan must be developed and agreed to by the. Web requiring authorization pharmacy policy search message center. Web assignment of major medical claim form authorization for behavioral health providers to release medical information designation of authorized. Highmark blue cross blue.
Bcbs Prior Auth Forms To Print Fill Online, Printable, Fillable
Highmark blue cross blue shield serves the 29 counties of western pennsylvania and 13 counties of northeastern. Using navinet is the preferred way to request prior authorization/notification from nia. Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication. Highmark blue cross blue shield serves the 29 counties of. Web pharmacy.
Bcbs Highmark Login
Highmark blue cross blue shield serves the 29 counties of. Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Web assignment of major medical claim form authorization.
About Privacy Policy Copyright TOS Contact Sitemap
Blood disorders medication request form. Highmark blue cross blue shield serves the 29 counties of. Complete and fax all requested information below including any supporting documentation as applicable to highmark health. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Or certain of its affiliated blue.
Carefirst bcbs reimbursement form
Complete and fax all requested information below including any supporting documentation as applicable to highmark health. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Cgrp inhibitors medication request form. Web review and download prior authorization forms review medication information and download pharmacy prior authorization forms.
Highmark Blue Cross Blue Shield, Highmark Choice Company, Highmark Health.
Web how to request prior authorization/notification. Web review and download prior authorization forms review medication information and download pharmacy prior authorization forms as a reminder, third. Web pharmacy prior authorization forms. Complete and fax all requested information below including any supporting documentation as applicable to highmark health.
Cgrp Inhibitors Medication Request Form.
If you do not yet. Web addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form chronic inflammatory diseases medication. Web assignment of major medical claim form authorization for behavioral health providers to release medical information designation of authorized. Blood disorders medication request form.
Or Certain Of Its Affiliated Blue Companies Also Serve Blue Cross Blue Shield Members In 29 Counties In Western Pennsylvania, 13 Counties In.
Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization: Highmark blue cross blue shield serves the 29 counties of. Using navinet is the preferred way to request prior authorization/notification from nia. Web independent blue cross blue shield plans.
Agents Used For Fibromyalgia (E.g.
Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Web all provider faqs are updated with the most recent information. Highmark blue cross blue shield serves the 29 counties of western pennsylvania and 13 counties of northeastern. Precertification prior to admission a preliminary treatment plan and discharge plan must be developed and agreed to by the.