Meridian Prior Auth Form
Meridian Prior Auth Form - To submit electronically, go to meridianrx.com and select “submit prior authorization.” Web welcome michigan complete members. Prior authorizations should be submitted through the new provider portal or via fax. Prior authorizations cannot be submitted over the phone. The following information is required for meridian to accept your authorization request: Please visit our new prior authorization website page to gain access to the secure portal and correct fax forms here. Web meridian prior (rx) authorization form. A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. • full name of member • member’s date of birth • member’s meridian id number
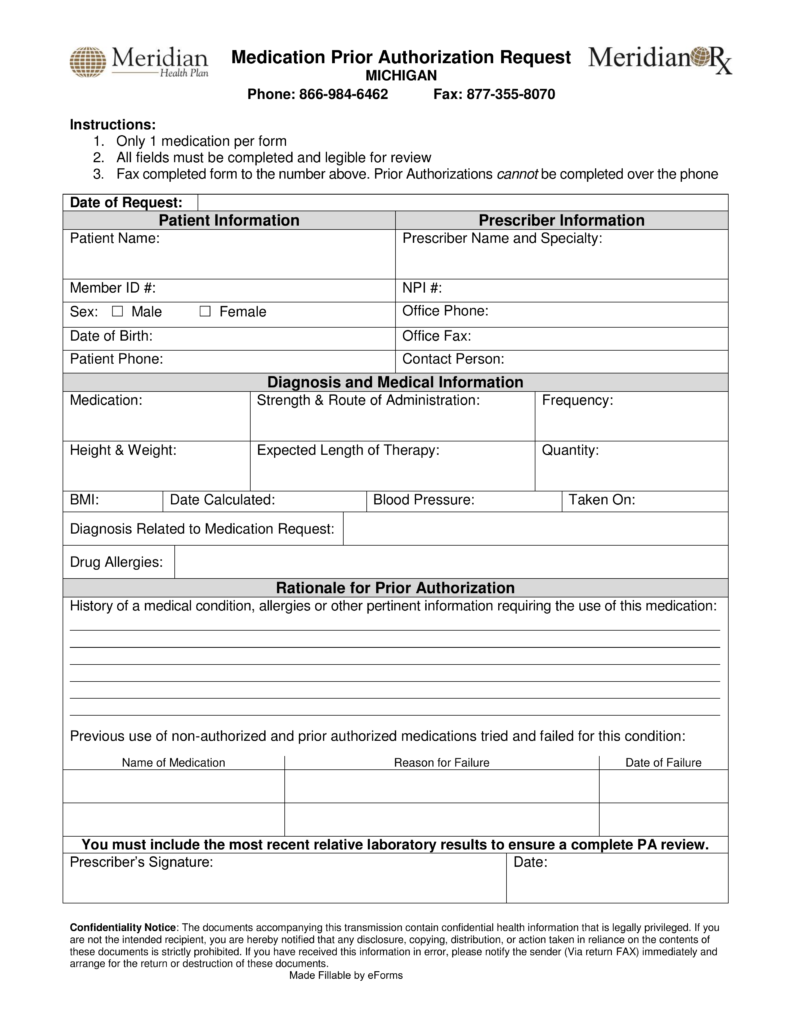
If an authorization is needed, you can access our login to submit online. Web meridian prior (rx) authorization form. Prior authorizations cannot be submitted over the phone. • full name of member • member’s date of birth • member’s meridian id number Web welcome michigan complete members. Web effective april 1, 2022, the electronic prior authorization (epa) form will no longer be an acceptable form of submission. Only 1 medication per form all fields must be completed and legible for review. Primary care provider reassignment form. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from.
If an authorization is needed, you can access our login to submit online. You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. Mobile crisis response provider reference guide. Weight watchers® exhausted benefit form Web meridian prior (rx) authorization form. To submit electronically, go to meridianrx.com and select “submit prior authorization.” Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Web effective april 1, 2022, the electronic prior authorization (epa) form will no longer be an acceptable form of submission. Primary care provider reassignment form. Web welcome michigan complete members.
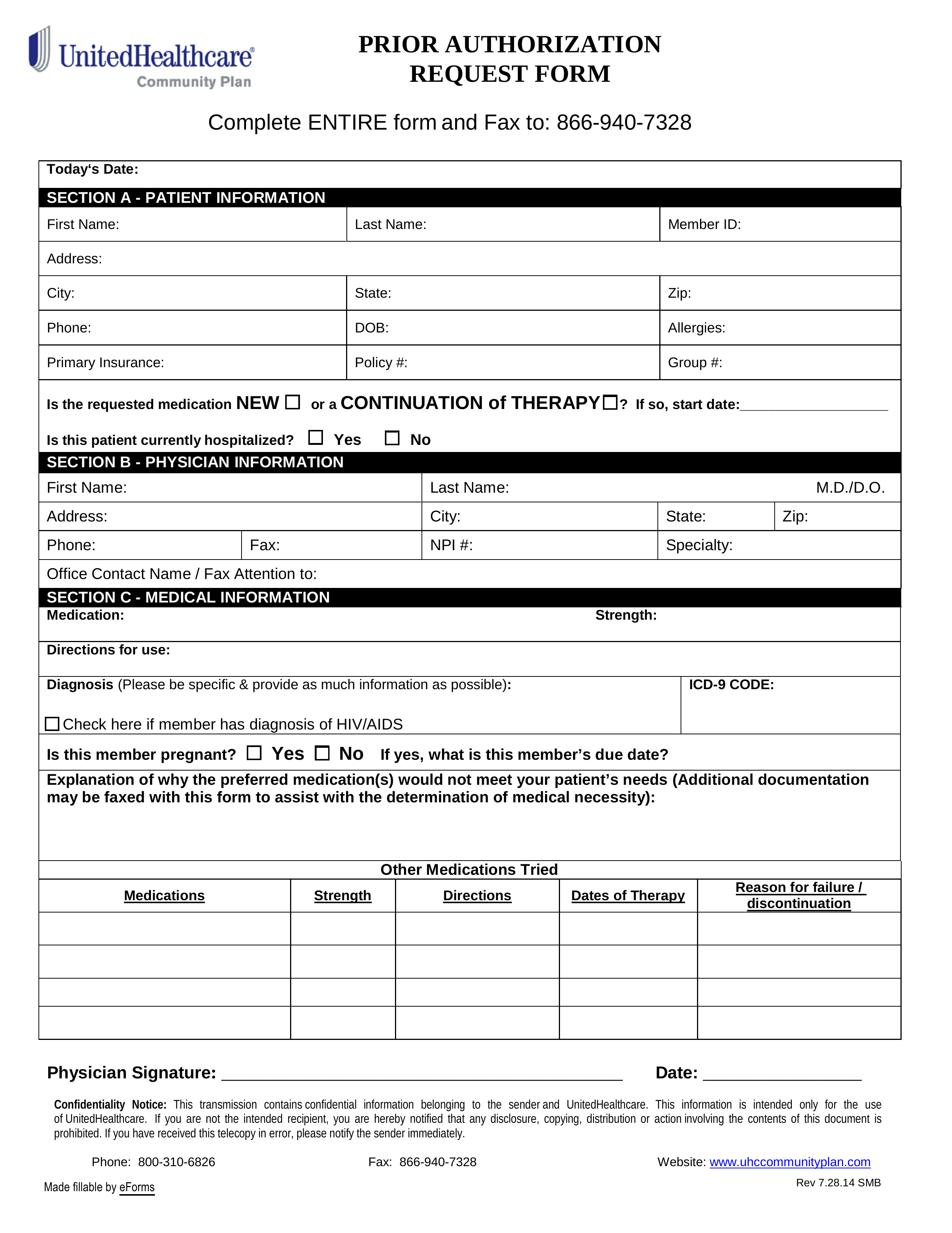
Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
The following information is required for meridian to accept your authorization request: Prior authorizations should be submitted through the new provider portal or via fax. Weight watchers® exhausted benefit form Mobile crisis response provider reference guide. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa).
Contact
You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. Web meridian prior (rx) authorization form. Weight watchers® exhausted benefit form Web effective april 1, 2022, the electronic prior authorization (epa) form will no longer be an acceptable form of submission. If an authorization is needed,.
Free Meridian Prior Prescription (Rx) Authorization Form PDF
Prior authorizations cannot be submitted over the phone. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. • full name of member • member’s date of.
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
The following information is required for meridian to accept your authorization request: Weight watchers® exhausted benefit form Web medication prior authorization request phone: A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. Web welcome michigan complete members.
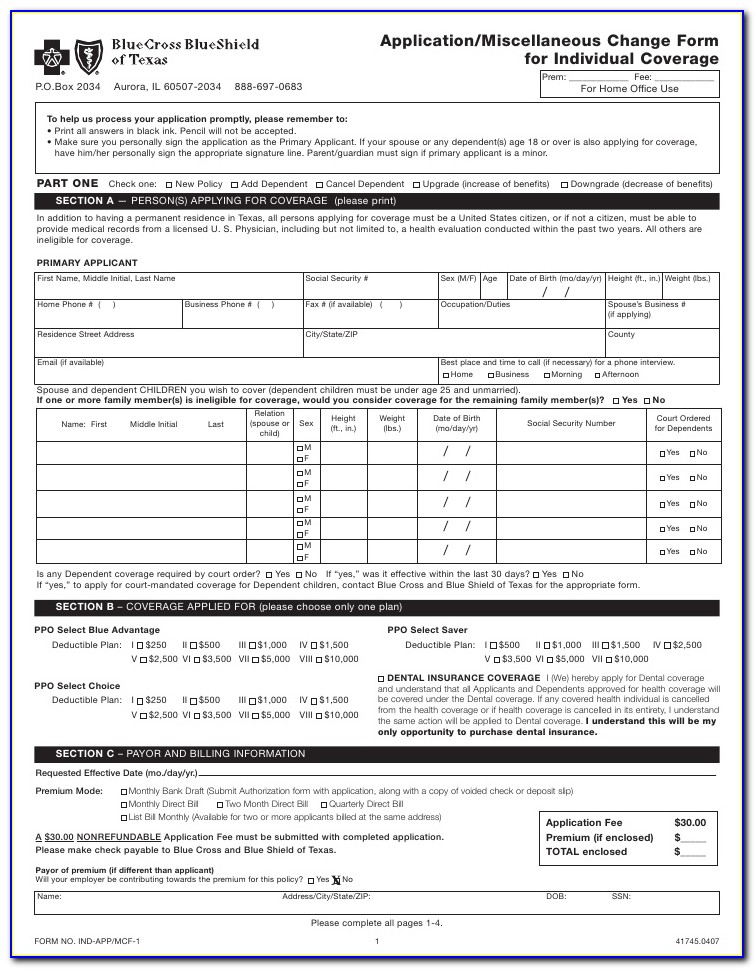
FREE 10+ Sample Medical Authorization Forms in PDF MS Word Excel
Prior authorizations cannot be submitted over the phone. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. Web effective april 1, 2022, the electronic prior.
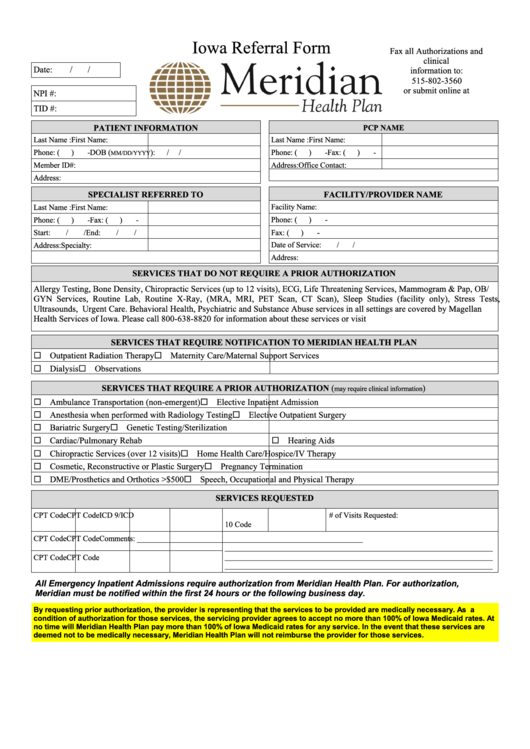
Fillable Iowa Referral Form Meridian Health Plan printable pdf download
Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web effective april 1, 2022, the electronic prior authorization (epa) form will no longer be an acceptable form of submission. Web welcome michigan complete members. Prior authorizations should be submitted through the new provider portal or via fax. Please visit.
Free Meridian Prior (Rx) Authorization Form PDF eForms
Prior authorizations cannot be submitted over the phone. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. • full name of member • member’s date of birth.
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Primary care provider reassignment form. Please visit our new prior authorization website page to gain access to the secure portal and correct fax forms here. Only 1 medication per form all fields must be completed and legible for review. Prior authorizations should be submitted through the new provider portal or via fax. • full name of member • member’s date.
Meridian Health Plan Medication Prior Authorization Form Illinois
Web meridian prior (rx) authorization form. Primary care provider reassignment form. Prior authorizations cannot be submitted over the phone. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web medication prior authorization request phone:
Michigan Information Meridian
Prior authorizations should be submitted through the new provider portal or via fax. Weight watchers® exhausted benefit form The following information is required for meridian to accept your authorization request: You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. Web effective april 1, 2022, the.
Web Prior Authorization Is Required Before Certain Services Are Rendered To Confirm Medical Necessity As Defined By The Member’s Plan.
A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. Prior authorizations should be submitted through the new provider portal or via fax. • full name of member • member’s date of birth • member’s meridian id number Primary care provider reassignment form.
Web Effective April 1, 2022, The Electronic Prior Authorization (Epa) Form Will No Longer Be An Acceptable Form Of Submission.
Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. To submit electronically, go to meridianrx.com and select “submit prior authorization.” Web welcome michigan complete members.
Web Meridian Prior (Rx) Authorization Form.
Prior authorizations cannot be submitted over the phone. Web medication prior authorization request phone: The following information is required for meridian to accept your authorization request: Weight watchers® exhausted benefit form
Mobile Crisis Response Provider Reference Guide.
Only 1 medication per form all fields must be completed and legible for review. Please visit our new prior authorization website page to gain access to the secure portal and correct fax forms here. If an authorization is needed, you can access our login to submit online.