Molina Pre Authorization Form
Molina Pre Authorization Form - Applied behavior analysis (aba) therapy prior authorization form. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: 2023 medicaid pa guide/request form effective 01/01/2023. Medicaid prior authorization annual review change log. If a request for services is denied, the requesting provider and the member will receive a Applied behavior analysis (aba) therapy level of. Prior authorization specialty medication request form. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Prior authorization/medication exception request form.
Medicaid prior authorization annual review change log. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. It is needed before you can get certain services or drugs. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. If a request for services is denied, the requesting provider and the member will receive a Edit, sign and save prior authorization req form. Web prior authorization lookup tool. Download or email molina & more fillable forms, register and subscribe now! Web home > members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
Prior authorization specialty medication request form. Applied behavior analysis (aba) therapy level of. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. 2023 medicaid pa guide/request form effective 01/01/2023. Molina healthcare of washington, inc. Medicaid prior authorization annual review change log. It is needed before you can get certain services or drugs. Please use the “find a provider” tool above, which features pdf versions of our provider directories. Web prior authorization lookup tool.
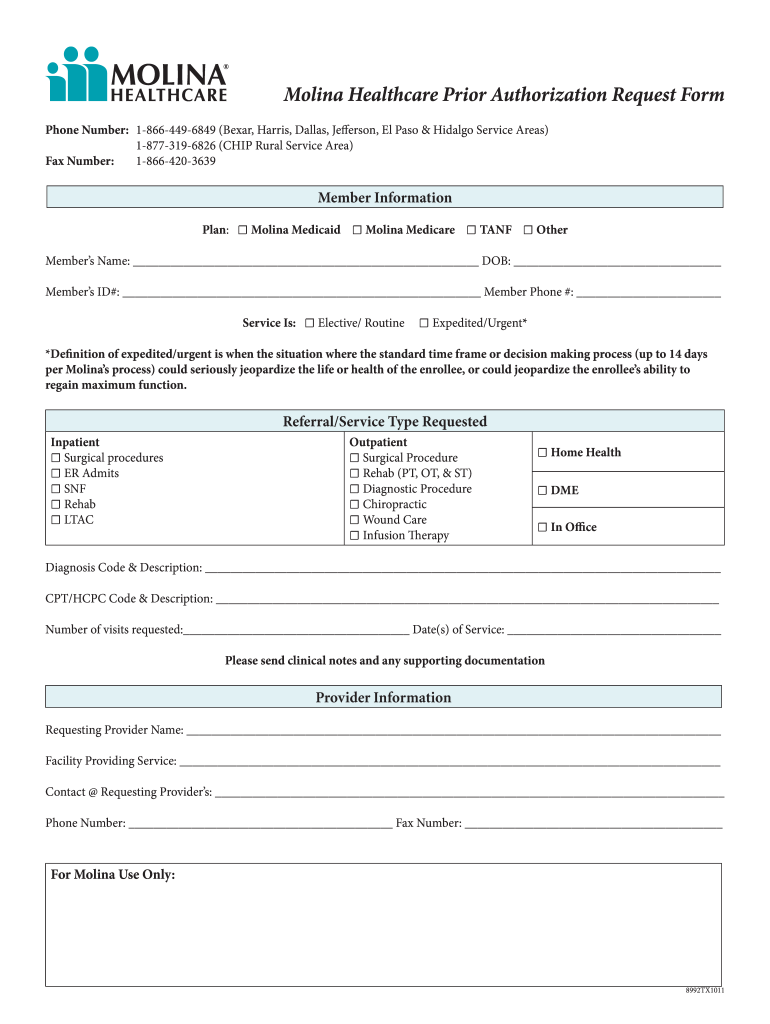
Molina Pre Authorization form Texas Unique Gi Edition Abteilung
Download or email molina & more fillable forms, register and subscribe now! If a request for services is denied, the requesting provider and the member will receive a Prior authorization/medication exception request form. Please use the “find a provider” tool above, which features pdf versions of our provider directories. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for.
WA Molina Healthcare Behavioral Health Authorization/Notification Form
Web home > members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Medicaid prior authorization annual review report. Prior authorization specialty medication request form. Download or email molina & more fillable forms, register and subscribe now! The fastest route for prior authorization is submission via fax.
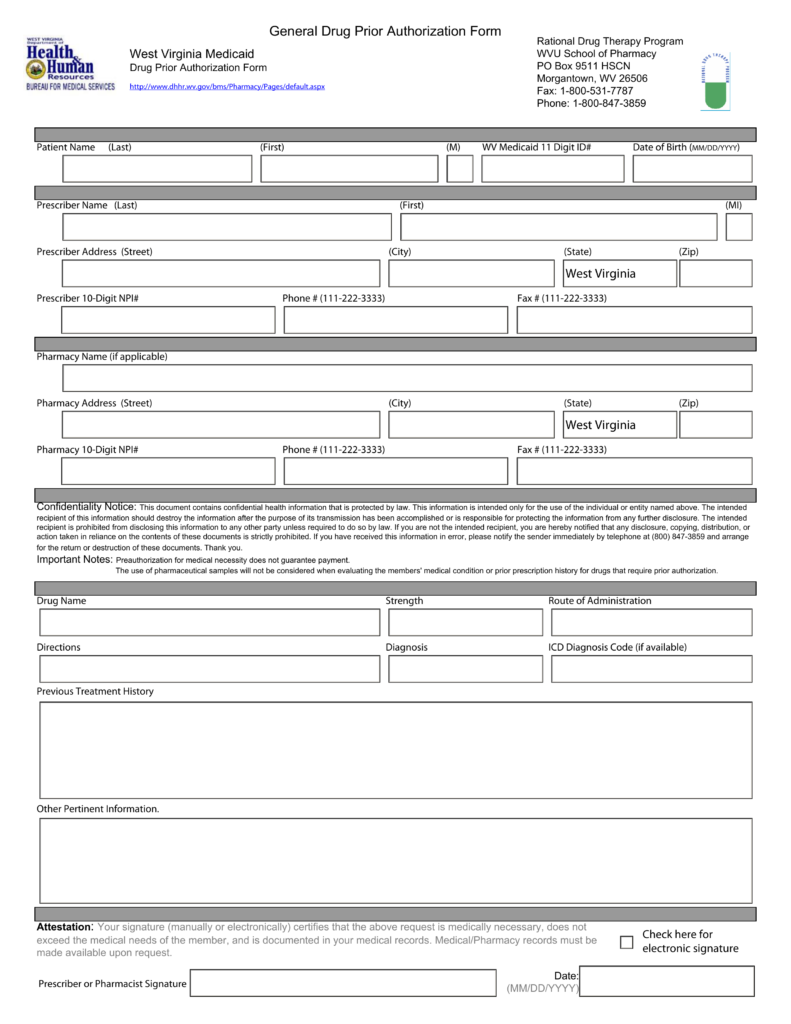
Free West Virginia Medicaid Prior (Rx) Authorization Form PDF
Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. It is needed before you can get certain services or drugs. The fastest route for prior authorization is submission via fax..
MOLINA HEALTHCARE, INC. FORM 8K EX99.1 September 16, 2011
If a request for services is denied, the requesting provider and the member will receive a Applied behavior analysis (aba) therapy prior authorization form. Medicaid prior authorization annual review report. The fastest route for prior authorization is submission via fax. Edit, sign and save prior authorization req form.
Medicare Id Card Sample Luxury Medicare Id Card Sample Awesome 8
Molina healthcare of washington, inc. Applied behavior analysis (aba) therapy level of. Edit, sign and save prior authorization req form. Prior authorization/medication exception request form. 2023 medicaid pa guide/request form effective 01/01/2023.
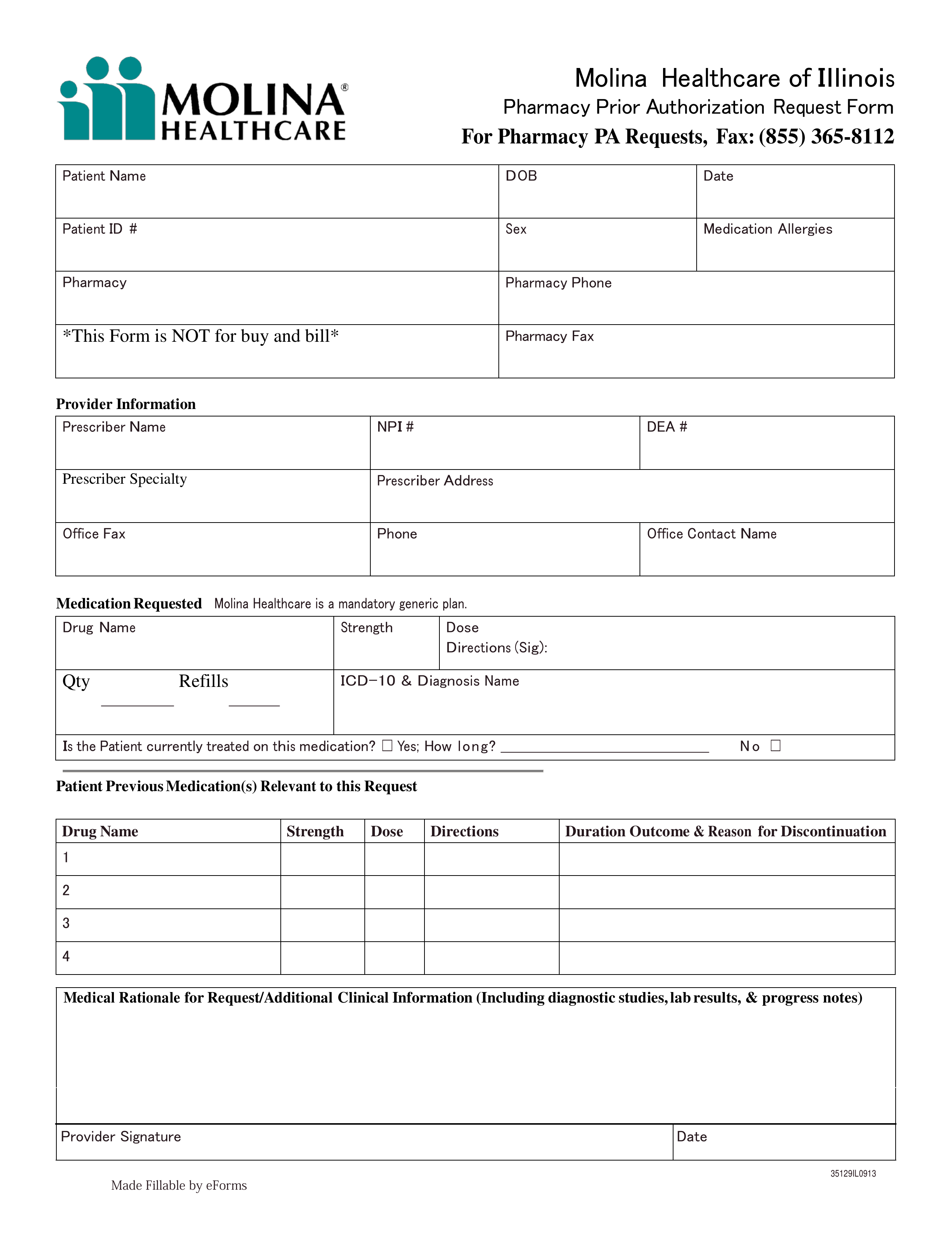
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Web prior authorization lookup tool. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Please use the “find a provider” tool above, which features pdf versions of our provider directories. Behavioral health admission notification/authorization request form. Molina healthcare of washington, inc.
Molina Pre Authorization form Texas Lovely Figure From Pharmacist and
If a request for services is denied, the requesting provider and the member will receive a Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Behavioral health admission notification/authorization request form. 2023 medicaid pa guide/request form effective 01/01/2023. Applied behavior analysis (aba) therapy level of.
Molina Medicare Pa Forms Universal Network
Applied behavior analysis (aba) therapy level of. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Molina healthcare of washington, inc. Please use the “find a provider” tool above, which features pdf versions of our provider directories. Web home > members > medicaid >.
Molina Pre Authorization form Texas Best Of Molina Healthcare Molina
Behavioral health admission notification/authorization request form. Prior authorization/medication exception request form. Web prior authorization lookup tool. Molina healthcare of washington, inc. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function.
Molina Prior Authorization Form 2021 Fill Online, Printable, Fillable
Medicaid prior authorization annual review report. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Applied behavior analysis (aba) therapy level of. • current (up to 6 months), adequate patient history related to the requested. If a request for services is denied, the requesting.
Applied Behavior Analysis (Aba) Therapy Prior Authorization Form.
It is needed before you can get certain services or drugs. Prior authorization specialty medication request form. Prior authorization/medication exception request form. If a request for services is denied, the requesting provider and the member will receive a
01/01/2022 For Dual Members With Medicaid, Please Refer To Your State Medicaid Pa Guide For Additional Pa Requirements Refer To Molina’s Provider Website Or Prior.
• current (up to 6 months), adequate patient history related to the requested. Download or email molina & more fillable forms, register and subscribe now! Please use the “find a provider” tool above, which features pdf versions of our provider directories. The fastest route for prior authorization is submission via fax.
Prior Authorization Is When Your Provider Gets Approval From Molina Healthcare To Provide You A Service.
Applied behavior analysis (aba) therapy level of. Behavioral health admission notification/authorization request form. Molina healthcare of washington, inc. Web home > members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations?
2023 Medicaid Pa Guide/Request Form (Vendors) Effective 07.01.2023 Important Information For Molina Healthcare Medicaid Providers Information Generally Required To Support Authorization Decision Making Includes:
Edit, sign and save prior authorization req form. Web molina healthcare prior authorization request form *the expedited/urgent service request designation should only be used if the treatment is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. 2023 medicaid pa guide/request form effective 01/01/2023. Medicaid prior authorization annual review change log.