Wellcare By Allwell Authorization Form
Wellcare By Allwell Authorization Form - This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by wellcare by allwell. Web authorization form expedited requests: Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Web what is the process for obtaining a prior authorization? Determination made as expeditiously as the enrollee’s Enrollment in our plans depends on contract renewal. The following information is generally required for all authorizations: We recommend that providers submit prior authorizations through the web portal, via phone or via fax. • when requesting a formulary exception, a drug coverage redeterminationform must be. Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor.
You may request prior authorization by contacting member services. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Web what is the process for obtaining a prior authorization? Web authorization form expedited requests: Complex imaging, mra, mri, pet and ct scans need to be verified by nia. Access key forms for authorizations, claims, pharmacy and more. • please refer to the formulary for specific types of exceptions. • when requesting a formulary exception, a drug coverage redeterminationform must be. Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Web a repository of medicare forms and documents for wellcare providers, covering topics such as authorizations, claims and behavioral health.
Musculoskeletal services need to be verified by turningpoint. • when requesting a formulary exception, a drug coverage redeterminationform must be. Web a repository of medicare forms and documents for wellcare providers, covering topics such as authorizations, claims and behavioral health. Complex imaging, mra, mri, pet and ct scans need to be verified by nia. Enrollment in our plans depends on contract renewal. We recommend that providers submit prior authorizations through the web portal, via phone or via fax. Web wellcare by allwell requires prior authorization (pa) as a condition of payment for many services. The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. You may request prior authorization by contacting member services.
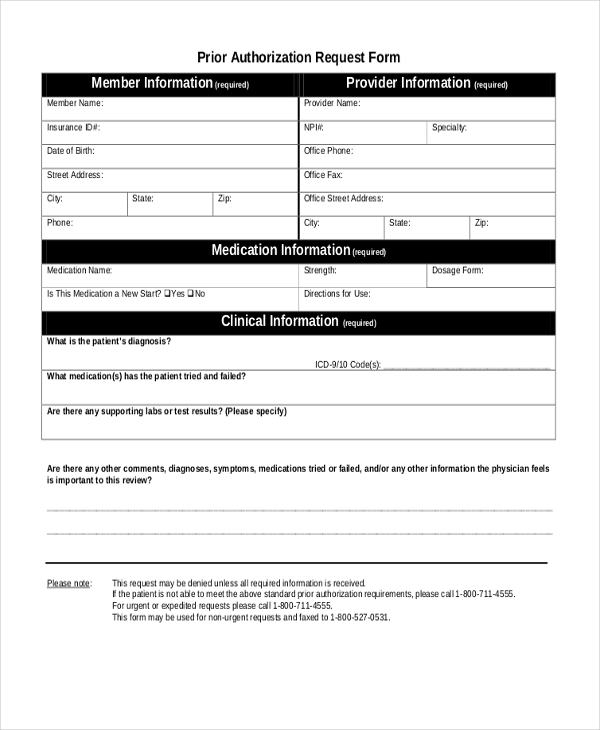
How To Submit Pre Authorization To Medicare
Determination made as expeditiously as the enrollee’s • when requesting a formulary exception, a drug coverage redeterminationform must be. Access key forms for authorizations, claims, pharmacy and more. This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by wellcare by allwell. The following information is generally required for all authorizations:
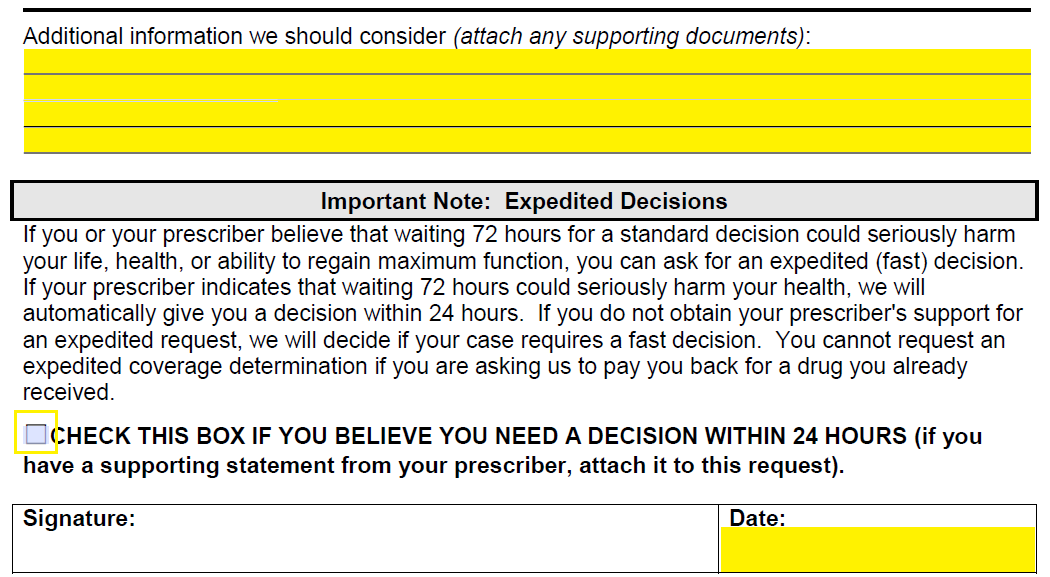
Unique Wellcare Medicaid Prior Authorization form MODELS
This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by wellcare by allwell. Musculoskeletal services need to be verified by turningpoint. Web authorization form expedited requests: Web a repository of medicare forms and documents for wellcare providers, covering topics such as authorizations, claims and behavioral health. • when requesting a formulary exception,.
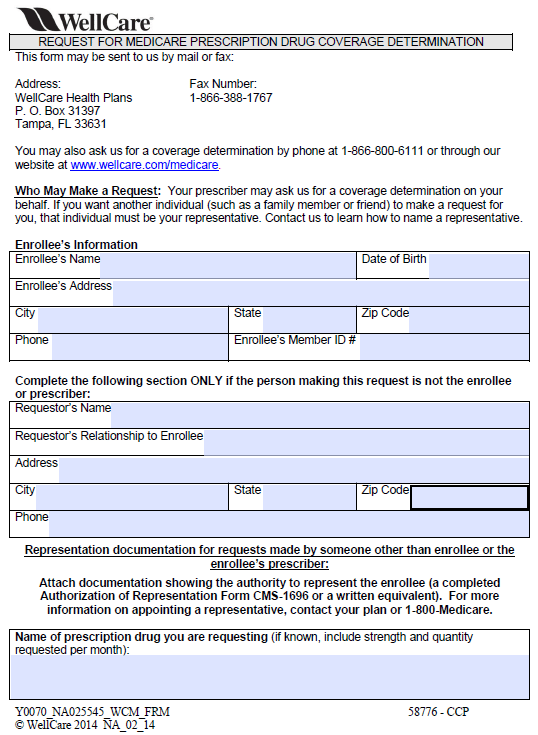
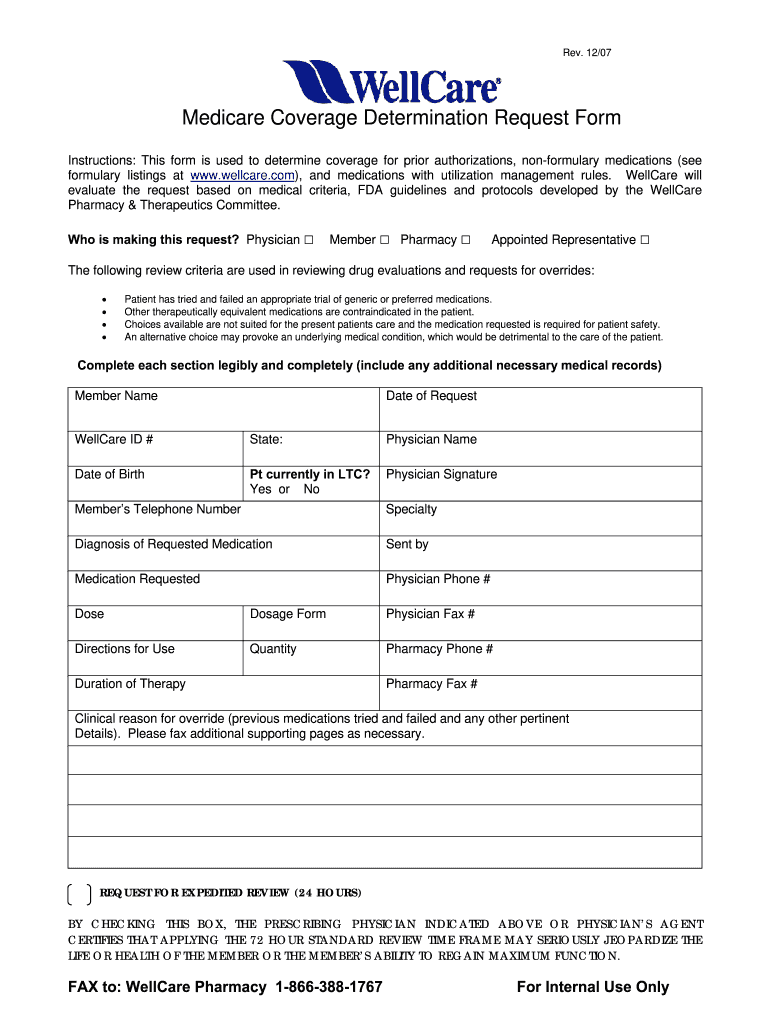
Free Wellcare Prior Prescription (Rx) Authorization Form PDF
We recommend that providers submit prior authorizations through the web portal, via phone or via fax. • when requesting a formulary exception, a drug coverage redeterminationform must be. Web what is the process for obtaining a prior authorization? This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by wellcare by allwell. Web.
Key.covermymeds Prior Authorization Form Form Resume Examples
• when requesting a formulary exception, a drug coverage redeterminationform must be. Web submitting an authorization request. The following information is generally required for all authorizations: Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Complex imaging, mra, mri, pet and ct scans need to be verified by nia.
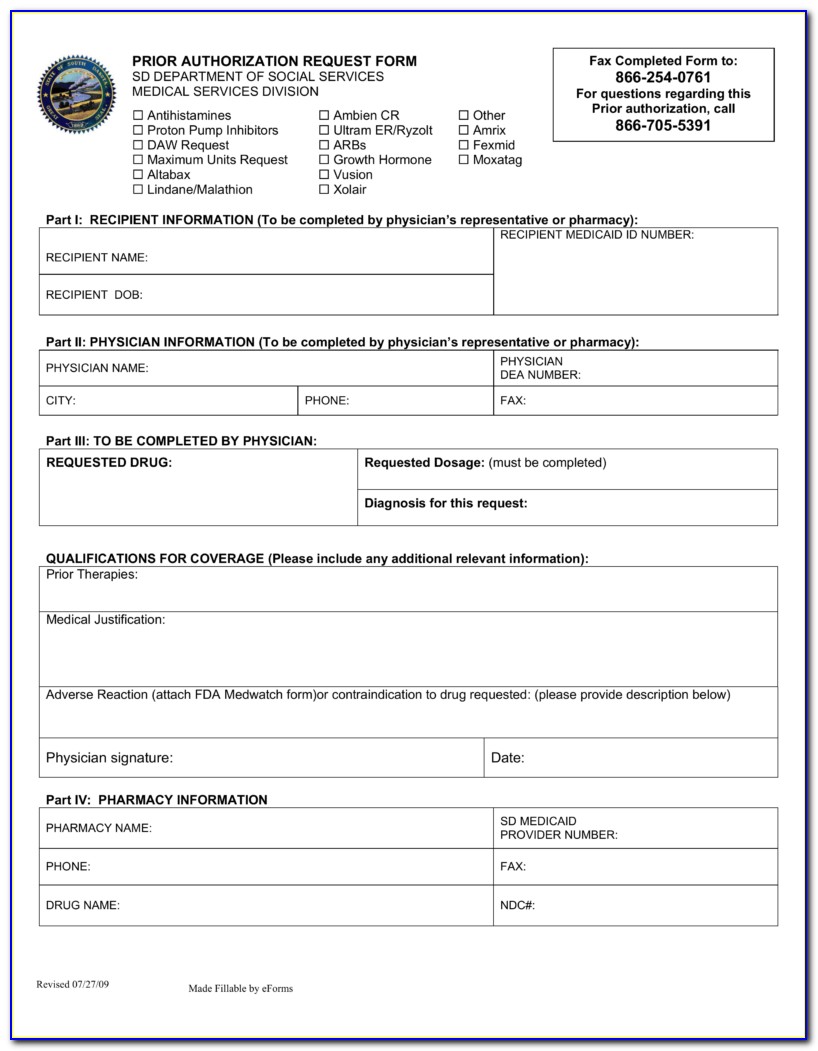
Wellcare Appeal Form Fill Out and Sign Printable PDF Template signNow
Musculoskeletal services need to be verified by turningpoint. Complex imaging, mra, mri, pet and ct scans need to be verified by nia. Web wellcare by allwell requires prior authorization (pa) as a condition of payment for many services. Web submitting an authorization request. Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a.
Anthem Medicare Advantage Disenrollment Form Form Resume Examples
Enrollment in our plans depends on contract renewal. Web wellcare by allwell requires prior authorization (pa) as a condition of payment for many services. Musculoskeletal services need to be verified by turningpoint. This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by wellcare by allwell. Web what is the process for obtaining.
FREE 10+ Sample Medicare Forms in PDF MS Word
Web what is the process for obtaining a prior authorization? We recommend that providers submit prior authorizations through the web portal, via phone or via fax. Web submitting an authorization request. This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by wellcare by allwell. Enrollment in our plans depends on contract renewal.
Wellcare Value Script Enrollment Form Form Resume Examples EZVgRlkYJk
The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only). Enrollment in our plans depends on contract renewal. Determination made as expeditiously as the enrollee’s Web submitting an authorization request. Web wellcare is the medicare brand for centene.
Wellcare Forms For Prior Authorization Fill Out and Sign Printable
Web wellcare by allwell requires prior authorization (pa) as a condition of payment for many services. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. The following information is generally required for all authorizations: • please refer to the formulary for specific types of exceptions. Access key forms for authorizations, claims,.
Wellcare Card 1 newacropol
Enrollment in our plans depends on contract renewal. Web submitting an authorization request. Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. • when requesting.
Determination Made As Expeditiously As The Enrollee’s
Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Web what is the process for obtaining a prior authorization? Web submitting an authorization request. Web a repository of medicare forms and documents for wellcare providers, covering topics such as authorizations, claims and behavioral health.
Web Authorization Form Expedited Requests:
Access key forms for authorizations, claims, pharmacy and more. • when requesting a formulary exception, a drug coverage redeterminationform must be. Web wellcare by allwell requires prior authorization (pa) as a condition of payment for many services. Complex imaging, mra, mri, pet and ct scans need to be verified by nia.
Enrollment In Our Plans Depends On Contract Renewal.
Musculoskeletal services need to be verified by turningpoint. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by wellcare by allwell. We recommend that providers submit prior authorizations through the web portal, via phone or via fax.
• Please Refer To The Formulary For Specific Types Of Exceptions.
The following information is generally required for all authorizations: You may request prior authorization by contacting member services. The fastest and most efficient way to request an authorization is through our secure provider portal, however you may also request an authorization via fax or phone (emergent or urgent authorizations only).